Is Dental Treatment Safe During Pregnancy?
/Now that we have addressed what oral changes to expect during pregnancy (see this post), let’s move on to dental treatment during pregnancy.
To answer the #1 question: YES, it is safe to have dental treatment done while pregnant. This includes exams, radiographs (x-rays), cleanings, fillings, root canals, and other treatment (even extractions).
The goals are to both maintain oral health during pregnancy to prevent any issues from progressing and to also decrease transmission of decay-causing bacteria to your baby.
The American College of Obstetricians and Gynecologists (ACOG) developed a Committee Opinion piece in which they stated, “Regular dental care is a key component to good oral and general health. Despite the lack of evidence that prenatal oral health care improves pregnancy outcomes, ample evidence shows that oral health care during pregnancy is safe and should be recommended to improve the oral and general health of the woman. Improved oral health of the woman may decrease transmission of potentially cariogenic bacteria to infants and reduce children’s future risk of caries.”
Let’s address a few specific aspects of dental treatment in more depth:
Radiographs (X-rays)
The concern with radiographs is always radiation exposure. Let me see if I can put things into proper perspective and allay any fears.
The accepted cumulative dose of ionizing radiation to a fetus during pregnancy is 5 rad. A single dental radiograph is 0.001 rad to the site of exposure (the pregnant mother’s mouth), so even less to the fetus with shielding.
A few authorities on the subject can say it better than I:
“No single diagnostic procedure results in a radiation dose that threatens the well-being of the developing embryo and fetus.“ — American College of Radiology
“[Fetal] risk is considered to be negligible at 5 rad or less when compared to the other risks of pregnancy, and the risk of malformations is significantly increased above control levels only at doses above 15 rad.” — National Council on Radiation Protection
“Women should be counseled that x-ray exposure from a single diagnostic procedure does not result in harmful fetal effects. Specifically, exposure to less than 5 rad has not been associated with an increase in fetal anomalies or pregnancy loss.” — American College of Obstetricians and Gynecologists
The decision making process for taking radiographs is a weighing between risk and benefit. As we’ve established, the risks of dental radiographs may be considered negligible. The benefits depend on your situation. If you’re experiencing a dental emergency (i.e. pain, dental trauma, infection), one or more dental radiographs may be necessary to properly diagnose and appropriately treat the issue. If you’re in for your routine cleaning and exam and have an excellent dental health record, you may opt to defer routine radiographs until after you have delivered your baby with little fear that decay is going undiagnosed.
Local Anesthetic (Numbing)
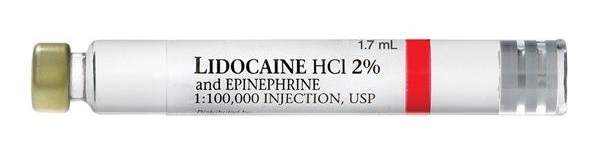
Lidocaine is one of the most common local anesthetics used in dentistry and it is a pregnancy category B drug. If you need to have a dental procedure done that requires local anesthetic, you can feel comfortable having lidocaine used for your appointment.
It is also important to note that dental local anesthetics also often contain epinephrine as a vasoconstrictor to enhance the anesthesia. The most common concentration of epinephrine with lidocaine is 1:100,000, or 0.01 mg/mL. Epinephrine is safe during pregnancy up to doses of 0.1 mg, as this does not adversely affect placental blood flow. The 1:100,000 concentration of epinephrine with a single dental lidocaine dose equals just 0.018 mg.
Supine Hypotensive Syndrome and Proper Positioning for Treatment
Supine hypotensive syndrome, also referred to as inferior vena cava compression syndrome, is caused when a pregnant woman is in a supine position (lying on her back) and the pregnant uterus compresses the inferior vena cava, leading to decreased venous return to the heart. This may lead to symptoms of dizziness, low blood pressure, pallor, sweating, nausea, and increased heart rate. Fortunately, supine hypotensive syndrome is easily avoided (or its symptoms readily resolved) with mindful positioning. If you are beyond 24 weeks pregnant and having dental work done, a pillow or rolled towel placed under your right side will prevent compression of your inferior vena cava. Alternatively, your dentist may opt to simply not recline your chair fully.
In closing:
Pregnancy is a time when caring for yourself is of utmost importance, and this includes your oral health. In years past, dentists were trained to avoid treating pregnant women unless absolutely necessary. Whenever possible, treatment was deferred until after delivery, and when treatment was done, it was typically limited to completion during the 2nd trimester of pregnancy. This thinking has become antiquated and physicians and dentists now encourage keeping to your dental care routine and recommend addressing dental needs as they arise. This is because the risk of treatment is low and treatment prevents issues from progressing and minimizes the risk of transmission of cariogenic bacteria from mother to baby.